Nutrition | Relevant Organ Systems
Overview of Relevant Organ Systems
The Digestive System
The process of digestion begins even before you put food into your mouth. When you feel hungry, your body sends a message to your brain that it is time to eat. Sights and smells influence your body’s preparedness for food. Smelling food sends a message to your brain. Your brain then tells the mouth to get ready, and you start to salivate in preparation for a meal.
Once you have eaten, your digestive system (Figure 2.4 “The Human Digestive System”) starts the process that breaks down the components of food into smaller components that can be absorbed and taken into the body. To do this, the digestive system functions on two levels, mechanically to move and mix ingested food and chemically to break down large molecules. The smaller nutrient molecules can then be absorbed and processed by cells throughout the body for energy or used as building blocks for new cells. The digestive system is one of the eleven organ systems of the human body, and it is composed of several hollow tube-shaped organs including the mouth, pharynx, esophagus, stomach, small intestine, large intestine (colon), rectum, and anus. It is lined with mucosal tissue that secretes digestive juices (which aid in the breakdown of food) and mucus (which facilitates the propulsion of food through the tract). Smooth muscle tissue surrounds the digestive tract and its contraction produces waves, known as peristalsis, that propel food down the tract. Nutrients, as well as some non-nutrients, are absorbed. Substances such as fiber get left behind and are appropriately excreted.
Figure 2.4 Digestion Breakdown of Macronutrients

Digestion converts components of the food we eat into smaller molecules that can be absorbed into the body and utilized for energy needs or as building blocks for making larger molecules in cells.
Figure 2.5 The Human Digestive System

Image by Allison Calabrese / CC BY 4.0
From the Mouth to the Stomach
There are four steps in the digestion process (Figure 2.5 “The Human Digestive System”). The first step is ingestion, which is the intake of food into the digestive tract. It may seem a simple process, but ingestion involves smelling food, thinking about food, and the involuntary release of saliva in the mouth to prepare for food entry. In the mouth, where the second step of digestion starts, the mechanical and chemical breakdown of food begins. The chemical breakdown of food involves enzymes, such as salivary amylase that starts the breakdown of large starch molecules into smaller components.
Mechanical breakdown starts with mastication (chewing) in the mouth. Teeth crush and grind large food particles, while saliva provides lubrication and enables food movement downward. The slippery mass of partially broken-down food is called a bolus, which moves down the digestive tract as you swallow. Swallowing may seem voluntary at first because it requires conscious effort to push the food with the tongue back toward the throat, but after this, swallowing proceeds involuntarily, meaning it cannot be stopped once it begins. As you swallow, the bolus is pushed from the mouth through the pharynx and into a muscular tube called the esophagus. As the bolus travels through the pharynx, a small flap called the epiglottis closes to prevent choking by keeping food from going into the trachea. Peristaltic contractions also known as peristalsis in the esophagus propel the food bolus down to the stomach (Figure 3.6 “Peristalsis in the Esophagus”). At the junction between the esophagus and stomach there is a sphincter muscle that remains closed until the food bolus approaches. The pressure of the food bolus stimulates the lower esophageal sphincter to relax and open and food then moves from the esophagus into the stomach. The mechanical breakdown of food is accentuated by the muscular contractions of the stomach and small intestine that mash, mix, slosh, and propel food down the alimentary canal. Solid food takes between four and eight seconds to travel down the esophagus, and liquids take about one second.
Figure 2.6 Peristalsis in the Esophagus

Image by Allison Calabrese / CC BY 4.0
From the Stomach to the Small Intestine
When food enters the stomach, a highly muscular organ, powerful peristaltic contractions help mash, pulverize, and churn food into chyme. Chyme is a semiliquid mass of partially digested food that also contains gastric juices secreted by cells in the stomach. These gastric juices contain hydrochloric acid and the enzyme pepsin, that chemically start breakdown of the protein components of food.
The length of time food spends in the stomach varies by the macronutrient composition of the meal. A high-fat or high-protein meal takes longer to break down than one rich in carbohydrates. It usually takes a few hours after a meal to empty the stomach contents completely into the small intestine.
The small intestine is divided into three structural parts: the duodenum, the jejunum, and the ileum. Once the chyme enters the duodenum (the first segment of the small intestine), the pancreas and gallbladder are stimulated and release juices that aid in digestion. The pancreas secretes up to 1.5 liters (.4 US gallons) of pancreatic juice through a duct into the duodenum per day. This fluid consists mostly of water, but it also contains bicarbonate ions that neutralize the acidity of the stomach-derived chyme and enzymes that further break down proteins, carbohydrates, and lipids. The gallbladder secretes a much smaller amount of a fluid called bile that helps to digest fats. Bile passes through a duct that joins the pancreatic ducts and is released into the duodenum. Bile is made in the liver and stored in the gall bladder. Bile’s components act like detergents by surrounding fats similar to the way dish soap removes grease from a frying pan. This allows for the movement of fats in the watery environment of the small intestine. Two different types of muscular contractions, called peristalsis and segmentation, control the movement and mixing of the food in various stages of digestion through the small intestine.
Similar to what occurs in the esophagus and stomach, peristalsis is circular waves of smooth muscle contraction that propel food forward. Segmentation from circular muscle contraction slows movement in the small intestine by forming temporary “sausage link” type of segments that allows chyme to slosh food back and forth in both directions to promote mixing of the chyme and enhance absorption of nutrients (Figure 2.7 “Segmentation”). Almost all the components of food are completely broken down to their simplest units within the first 25 centimeters of the small intestine. Instead of proteins, carbohydrates, and lipids, the chyme now consists of amino acids, monosaccharides, and emulsified components of triglycerides.
Figure 2.7 Segmentation

“Segmentation” by OpenStax College / CC BY 3.0
The third step of digestion (nutrient absorption) takes place mainly in the remaining length of the small intestine, or ileum (> 5 meters). The way the small intestine is structured gives it a huge surface area to maximize nutrient absorption. The surface area is increased by folds, villi, and microvilli. Digested nutrients are absorbed into either capillaries or lymphatic vessels contained within each microvillus.
The small intestine is perfectly structured for maximizing nutrient absorption. Its surface area is greater than 200 square meters, which is about the size of a tennis court. The large surface area is due to the multiple levels of folding. The internal tissue of the small intestine is covered in villi, which are tiny finger-like projections that are covered with even smaller projections, called microvilli (Figure 2.8 “Structure of the Small Intestine”). The digested nutrients pass through the absorptive cells of the intestine via diffusion or special transport proteins. Amino acids, short fatty acids, and monosaccharides (sugars) are transported from the intestinal cells into capillaries, but the larger fatty acids, fat-soluble vitamins, and other lipids are transported first through lymphatic vessels, which soon meet up with blood vessels.
Figure 2.8 Structure of the Small Intestine
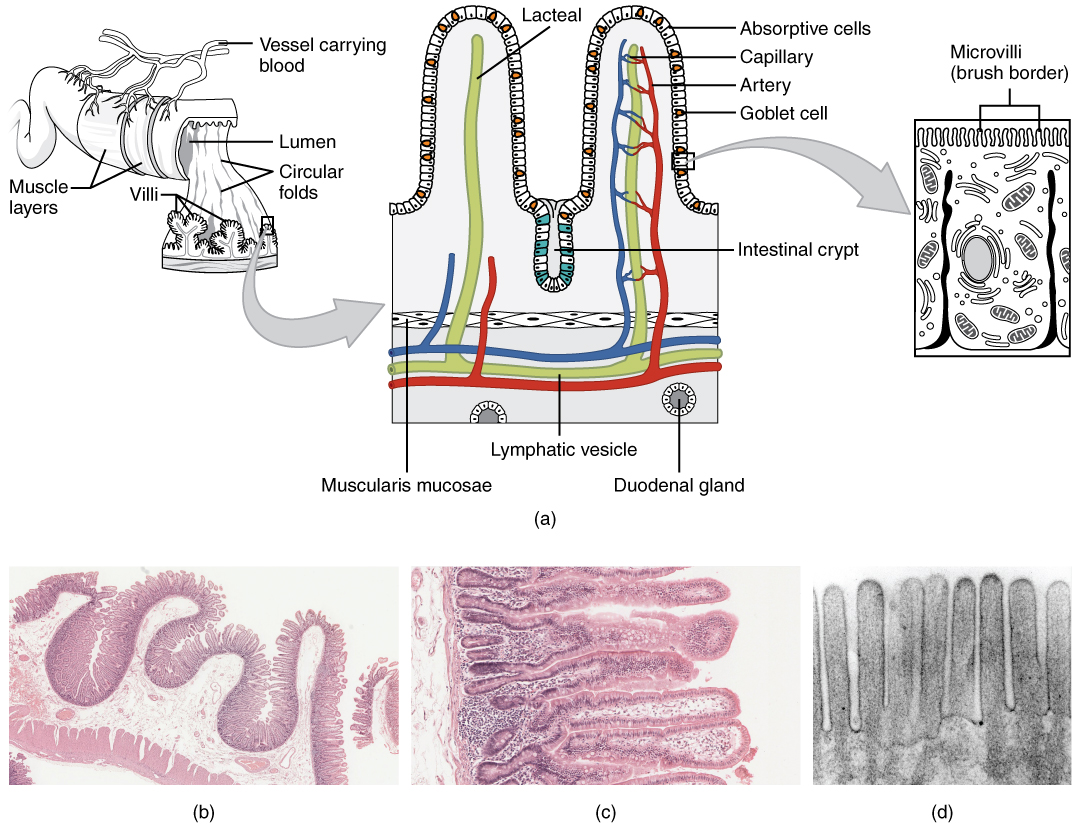
“Histology Small Intestines” by OpenStax College / CC BY 3.0
From the Small Intestine to the Large Intestine
The process of digestion is fairly efficient. Any food that is still incompletely broken down (usually less than ten percent of food consumed) and the food’s indigestible fiber content move from the small intestine to the large intestine (colon) through a connecting valve. A main task of the large intestine is to absorb much of the remaining water. Remember, water is present not only in solid foods and beverages, but also the stomach releases a few hundred milliliters of gastric juice, and the pancreas adds approximately 500 milliliters during the digestion of the meal. For the body to conserve water, it is important that excessive water is not lost in fecal matter. In the large intestine, no further chemical or mechanical breakdown of food takes place unless it is accomplished by the bacteria that inhabit this portion of the intestinal tract. The number of bacteria residing in the large intestine is estimated to be greater than 1014, which is more than the total number of cells in the human body (1013). This may seem rather unpleasant, but the great majority of bacteria in the large intestine are harmless and many are even beneficial.
There has been significant talk about pre- and probiotic foods in the mainstream media. The World Health Organization defines probiotics as live bacteria that confer beneficial health effects on their host. They are sometimes called “friendly bacteria.” The most common bacteria labeled as probiotic is lactic acid bacteria (lactobacilli). They are added as live cultures to certain fermented foods such as yogurt. Prebiotics are indigestible foods, primarily soluble fibers, that stimulate the growth of certain strains of bacteria in the large intestine and provide health benefits to the host.
Expert nutritionists agree that more health benefits of pre- and probiotics will likely reach scientific consensus. As the fields of pre- and probiotic manufacturing and their clinical study progress, more information on proper dosing and what exact strains of bacteria are potentially “friendly” will become available.
From the Large Intestine to the Anus
After a few hours in the stomach, plus three to six hours in the small intestine, and about sixteen hours in the large intestine, the digestion process enters step four, which is the elimination of indigestible food matter as feces. Feces contain indigestible food components and gut bacteria (almost 50 percent of content). It is stored in the rectum until it is expelled through the anus via defecation.
Nutrients are Essential for Cell and Organ Function
When the digestive system has broken down food to its nutrient components, the body eagerly awaits delivery. Water soluble nutrients absorbed into the blood travel directly to the liver via a major blood vessel called the portal vein. One of the liver’s primary functions is to regulate metabolic homeostasis. Metabolic homeostasis is achieved when the nutrients consumed and absorbed match the energy required to carry out life’s biological processes. Simply put, nutrient energy intake equals energy output. Whereas glucose and amino acids are directly transported from the small intestine to the liver, lipids are transported to the liver by a more circuitous route involving the lymphatic system. The lymphatic system is a one-way system of vessels that transports lymph, a fluid rich in white blood cells, and lipid soluble substances after a meal containing lipids. The lymphatic system slowly moves its contents through the lymphatic vessels and empties into blood vessels in the upper chest area. Now, the absorbed lipid soluble components are in the blood where they can be distributed throughout the body and utilized by cells (see Figure 2.9 “The Absorption of Nutrients”).
Figure 2.9 The Absorption of Nutrients

Image by Allison Calabrese / CC BY 4.0
Maintaining the body’s energy status quo is crucial because when metabolic homeostasis is disturbed by an eating disorder or disease, bodily function suffers. The liver is the only organ in the human body that is capable of exporting nutrients for energy production to other tissues. Therefore, when a person is in between meals (fasted state) the liver exports nutrients, and when a person has just eaten (fed state) the liver stores nutrients within itself. Nutrient levels and the hormones that respond to their levels in the blood provide the input so that the liver can distinguish between the fasted and fed states and distribute nutrients appropriately. Although not considered to be an organ, adipose tissue stores fat in the fed state and mobilizes fat components to supply energy to other parts of the body when energy is needed.
All eleven organ systems in the human body require nutrient input to perform their specific biological functions. Overall health and the ability to carry out all of life’s basic processes is fueled by energy-supplying nutrients (carbohydrate, fat, and protein). Without them, organ systems would fail, humans would not reproduce, and the race would disappear. In this section, we will discuss some of the critical nutrients that support specific organ system functions.
The Cardiovascular System

“Simplified diagram of the human Circulatory system in anterior view” by Mariana Ruiz / Public Domain
The cardiovascular system is one of the eleven organ systems of the human body. Its main function is to transport nutrients to cells and wastes from cells (Figure 2.12 “Cardiovascular Transportation of Nutrients”). This system consists of the heart, blood, and blood vessels. The heart pumps the blood, and the blood is the transportation fluid. The transportation route to all tissues, a highly intricate blood-vessel network, comprises arteries, veins, and capillaries. Nutrients absorbed in the small intestine travel mainly to the liver through the hepatic portal vein. From the liver, nutrients travel upward through the inferior vena cava blood vessel to the heart. The heart forcefully pumps the nutrient-rich blood first to the lungs to pick up some oxygen and then to all other cells in the body. Arteries become smaller and smaller on their way to cells, so that by the time blood reaches a cell, the artery’s diameter is extremely small and the vessel is now called a capillary. The reduced diameter of the blood vessel substantially slows the speed of blood flow. This dramatic reduction in blood flow gives cells time to harvest the nutrients in blood and exchange metabolic wastes.
Figure 2.11 The Blood Flow in the Cardiovascular System
 “Blood Flow Through the Heart” by OpenStax College / CC BY 3.0
“Blood Flow Through the Heart” by OpenStax College / CC BY 3.0
Blood’s Function in the Body and in Metabolism Support
You know you cannot live without blood, and that your heart pumps your blood over a vast network of veins and arteries within your body, carrying oxygen to your cells. However, beyond these basic facts, what do you know about your blood?
Blood transports absorbed nutrients to cells and waste products from cells. It supports cellular metabolism by transporting synthesized macromolecules from one cell type to another and carrying waste products away from cells. Additionally, it transports molecules, such as hormones, allowing for communication between organs. The volume of blood coursing throughout an adult human body is about 5 liters (1.3 US gallons) and accounts for approximately 8 percent of human body weight.
Blood Components and Support of Blood Function
Blood is about 78 percent water and 22 percent solids by volume. The liquid part of blood is called plasma and it is mostly water (95 percent), but also contains proteins, ions, glucose, lipids, vitamins, minerals, waste products, gases, enzymes, and hormones. We have learned that the protein albumin is found in high concentrations in the blood. Albumin helps maintain fluid balance between blood and tissues, as well as helping to maintain a constant blood pH. We have also learned that the water component of blood is essential for its actions as a transport vehicle, and that the electrolytes carried in blood help to maintain fluid balance and a constant pH. Furthermore, the high water content of blood helps maintain body temperature, and the constant flow of blood distributes heat throughout the body. Blood is exceptionally good at temperature control, so much so that the many small blood vessels in your nose are capable of warming frigid air to body temperature before it reaches the lungs.
The cellular components of blood include red blood cells, white blood cells, and platelets. Red blood cells are the most numerous of the components. Each drop of blood contains millions of them. Red blood cells are red because they each contain approximately 270 million hemoglobin proteins, which contain the mineral iron, which turns red when bound to oxygen. The most vital duty of red blood cells is to transport oxygen from the lungs to all cells in the body so that cells can utilize oxygen to produce energy via aerobic metabolism. The white blood cells that circulate in blood are part of the immune system, and they survey the entire body looking for foreign invaders to destroy. They make up about 1 percent of blood volume. Platelets are fragments of cells that are always circulating in the blood in case of an emergency. When blood vessels are injured, platelets rush to the site of injury to plug the wound. Blood is under a constant state of renewal and is synthesized from stem cells residing in bone marrow. Red blood cells live for about 120 days, white blood cells live anywhere from eighteen hours to one year, or even longer, and platelets have a lifespan of about ten days.
Figure 2.12 Cardiovascular Transportation of Nutrients

The cardiovascular system transports nutrients to all cells and carries wastes out.
Nutrients In
Once absorbed from the small intestine, all nutrients require transport to cells in need of their support. Additionally, molecules manufactured in other cells sometimes require delivery to other organ systems. Blood is the conduit and blood vessels are the highway that support nutrient and molecule transport to all cells. Water-soluble molecules, such as some vitamins, minerals, sugars, and many proteins, move independently in blood. Fat-soluble vitamins, triglycerides, cholesterol, and other lipids are packaged into lipoproteins that allow for transport in the watery milieu of blood. Many proteins, drugs, and hormones are dependent on transport carriers, primarily by the plasma protein albumin. In addition to transporting all of these molecules, blood transfers oxygen taken in by the lungs to all cells in the body. As discussed, the iron-containing hemoglobin molecule in red blood cells serves as the oxygen carrier.
Waste Out
In the metabolism of macronutrients to energy, cells produce the waste products carbon dioxide and water. As blood travels through smaller and smaller vessels, the rate of blood flow is dramatically reduced, allowing for efficient exchange of nutrients and oxygen for cellular waste products through tiny capillaries. The kidneys remove any excess water from the blood, and blood delivers the carbon dioxide to the lungs where it is exhaled. Also, the liver produces the waste product urea from the breakdown of amino acids and detoxifies many harmful substances, all of which require transport in the blood to the kidneys for excretion.
Interdependance
The eleven organ systems in the body completely depend on each other for continued survival as a complex organism. Blood allows for transport of nutrients, wastes, water, and heat, and is also a conduit of communication between organ systems. Blood’s importance to the rest of the body is aptly presented in its role in glucose delivery, especially to the brain. The brain metabolizes, on average, 6 grams of glucose per hour. In order to avert confusion, coma, and death, glucose must be readily available to the brain at all times. To accomplish this task, cells in the pancreas sense glucose levels in the blood. If glucose levels are low, the hormone glucagon is released into the blood and is transported to the liver where it communicates the signal to ramp-up glycogen breakdown and glucose synthesis. The liver does just that, and glucose is released into the blood, which transports it to the brain. Concurrently, blood transports oxygen to support the metabolism of glucose to provide energy in the brain. Healthy blood conducts its duties rapidly, avoiding hypoglycemic coma and death.
Measuring Blood Contents
Since blood is the conduit of metabolic products and wastes, measuring the components of blood, and particular substances in blood, can reveal not only the health of blood, but also the health of other organ systems. In standard blood tests performed during an annual physical, the typical blood tests conducted can tell your physician about the functioning of a particular organ or about disease risk.
A biomarker is defined as a measurable molecule or trait that is connected with a specific disease or health condition. The concentrations of biomarkers in blood are indicative of disease risk. Some biomarkers are cholesterol, triglycerides, glucose, and prostate-specific antigen. The results of a blood test give the concentrations of substances in a person’s blood and display the normal ranges for a certain population group. Many factors, such as physical activity level, diet, alcohol intake, and medicine intake can influence a person’s blood-test levels and cause them to fall outside the normal range, so results of blood tests outside the “normal” range are not always indicative of health problems. The assessment of multiple blood parameters aids in the diagnosis of disease risk and is indicative of overall health status. See Table 2.2 “Blood Tests” for a partial list of substances measured in a typical blood test. This table notes only a few of the things that their levels tell us about health.
Table 2.2 Blood Tests
| Substance Measured | Indicates |
| Red-blood-cell count | Oxygen-carrying capacity |
| Hematocrit (red-blood-cell volume) | Anemia risk |
| White-blood-cell count | Presence of infection |
| Platelet count | Bleeding disorders, atherosclerosis risk |
| pH | Metabolic, kidney, respiratory abnormalities |
| Albumin | Liver, kidney, and Crohn’s disease, dehydration, protein deficiency |
| Bilirubin | Liver-function abnormality |
| Oxygen/Carbon Dioxide | Respiratory or metabolic abnormality |
| Hemoglobin | Oxygen-carrying capacity |
| Iron | Anemia risk |
| Magnesium | Magnesium deficiency |
| Electrolytes (calcium, chloride, magnesium, potassium) | Many illnesses (kidney, metabolic, etc.) |
| Cholesterol | Cardiovascular disease risk |
| Triglycerides | Cardiovascular disease risk |
| Glucose | Diabetes risk |
| Hormones | Many illnesses (diabetes, reproductive abnormalities) |
The Endocrine System
Figure 2.19 The Endocrine System
What is the causal relationship between over-nutrition and Type 2 diabetes? The prevailing theory is that the overconsumption of high-fat and high-sugar foods causes changes in muscle, fat, and liver cells that leads to a diminished response from the pancreatic hormone insulin. These cells are called “insulin-resistant.” Insulin is released after a meal and instructs the liver and other tissues to take up glucose and fatty acids that are circulating in the blood. When cells are resistant to insulin they do not take up enough glucose and fatty acids, so glucose and fatty acids remain at high concentrations in the blood. The chronic elevation of glucose and fatty acids in the blood also causes damage to other tissues over time, so that people who have Type 2 diabetes are at increased risk for cardiovascular disease, kidney disease, nerve damage, and eye disease.
The Urinary System
The urinary system has roles you may be well aware of: cleansing the blood and ridding the body of wastes probably come to mind. However, there are additional, equally important functions played by the system. Take for example, regulation of pH, a function shared with the lungs and the buffers in the blood. Additionally, the regulation of blood pressure is a role shared with the heart and blood vessels. What about regulating the concentration of solutes in the blood? Did you know that the kidney is important in determining the concentration of red blood cells? Eighty-five percent of the erythropoietin (EPO) produced to stimulate red blood cell production is produced in the kidneys. The kidneys also perform the final synthesis step of vitamin D production, converting calcidiol to calcitriol, the active form of vitamin D.
If the kidneys fail, these functions are compromised or lost altogether, with devastating effects on homeostasis. The affected individual might experience weakness, lethargy, shortness of breath, anemia, widespread edema (swelling), metabolic acidosis, rising potassium levels, heart arrhythmias, and more. Each of these functions is vital to your well-being and survival. The urinary system, controlled by the nervous system, also stores urine until a convenient time for disposal and then provides the anatomical structures to transport this waste liquid to the outside of the body. Failure of nervous control or the anatomical structures leading to a loss of control of urination results in a condition called incontinence.
Characteristics of the urine change, depending on influences such as water intake, exercise, environmental temperature, nutrient intake, and other factors . Some of the characteristics such as color and odor are rough descriptors of your state of hydration. For example, if you exercise or work outside, and sweat a great deal, your urine will turn darker and produce a slight odor, even if you drink plenty of water. Athletes are often advised to consume water until their urine is clear. This is good advice; however, it takes time for the kidneys to process body fluids and store it in the bladder. Another way of looking at this is that the quality of the urine produced is an average over the time it takes to make that urine. Producing clear urine may take only a few minutes if you are drinking a lot of water or several hours if you are working outside and not drinking much.
Figure 2.20 Urine Color
Urine volume varies considerably. The normal range is one to two liters per day. The kidneys must produce a minimum urine volume of about 500 mL/day to rid the body of wastes. Output below this level may be caused by severe dehydration or renal disease and is termed oliguria. The virtual absence of urine production is termed anuria. Excessive urine production is polyuria, which may occur in diabetes mellitus when blood glucose levels exceed the filtration capacity of the kidneys and glucose appears in the urine. The osmotic nature of glucose attracts water, leading to increased water loss in the urine.
Urine is a fluid of variable composition that requires specialized structures to remove it from the body safely and efficiently. Blood is filtered, and the filtrate is transformed into urine at a relatively constant rate throughout the day. This processed liquid is stored until a convenient time for excretion. All structures involved in the transport and storage of the urine are large enough to be visible to the naked eye. This transport and storage system not only stores the waste, but it protects the tissues from damage due to the wide range of pH and osmolarity of the urine, prevents infection by foreign organisms, and for the male, provides reproductive functions. The urinary bladder collects urine from both ureters (Figure 2.21 “Urinary System Location”).
Figure 2.21 Urinary System Location
Figure 2.22 The Bladder
The kidneys lie on either side of the spine in the retroperitoneal space behind the main body cavity that contains the intestines. The kidneys are well protected by muscle, fat, and the lower ribs. They are roughly the size of your fist, and the male kidney is typically a bit larger than the female kidney. The kidneys are well vascularized, receiving about 25 percent of the cardiac output at rest.
Figure 2.23 The Kidneys
The kidneys (as viewed dorsally; from the back of the body) are slightly protected by the ribs and are surrounded by fat for protection (not shown).
The effects of failure of parts of the urinary system may range from inconvenient (incontinence) to fatal (loss of filtration and many other functions). The kidneys catalyze the final reaction in the synthesis of active vitamin D that in turn helps regulate Ca2+. The kidney hormone EPO stimulates erythrocyte development and promotes adequate O2 transport. The kidneys help regulate blood pressure through Na+ and water retention and loss. The kidneys work with the adrenal cortex, lungs, and liver in the renin–angiotensin–aldosterone system to regulate blood pressure. They regulate osmolarity of the blood by regulating both solutes and water. Three electrolytes are more closely regulated than others: Na+, Ca2+, and K+. The kidneys share pH regulation with the lungs and plasma buffers, so that proteins can preserve their three-dimensional conformation and thus their function.
The Skeletal System
Bone Structure and Function
Your bones are stronger than reinforced concrete. Bone tissue is a composite of fibrous strands of collagen (a type of protein) that resemble the steel rebar in concrete and a hardened mineralized matrix that contains large amounts of calcium, just like concrete. But this is where the similarities end. Bone outperforms reinforced concrete by several orders of magnitude in compression and tension strength tests. Why? The microarchitecture of bone is complex and built to withstand extreme forces. Moreover, bone is a living tissue that is continuously breaking down and forming new bone to adapt to mechanical stresses.
The Skeletal System in short
The human skeleton consists of 206 bones and other connective tissues called ligaments, tendons, and cartilage. Ligaments connect bones to other bones, tendons connect bones to muscles, and cartilage provides bones with more flexibility and acts as a cushion in the joints between bones. The skeleton’s many bones and connective tissues allow for multiple types of movement such as typing and running. The skeleton provides structural support and protection for all the other organ systems in the body. The skull, or cranium, is like a helmet and protects the eyes, ears, and brain. The ribs form a cage that surrounds and protects the lungs and heart. In addition to aiding in movement, protecting organs, and providing structural support, red and white blood cells and platelets are synthesized in bone marrow. Another vital function of bones is that they act as a storage depot for minerals such as calcium, phosphorous, and magnesium. Although bone tissue may look inactive at first glance, at the microscopic level you will find that bones are continuously breaking down and reforming. Bones also contain a complex network of canals, blood vessels, and nerves that allow for nutrient transport and communication with other organ systems.
Figure 2.25 Human Skeletal Structure
Bone Anatomy and Structure
To optimize bone health through nutrition, it is important to understand bone anatomy. The skeleton is composed of two main parts, the axial and the appendicular parts. The axial skeleton consists of the skull, vertebral column, and rib cage, and is composed of eighty bones. The appendicular skeleton consists of the shoulder girdle, pelvic girdle, and upper and lower extremities, and is composed of 126 bones. Bones are also categorized by size and shape. There are four types of bone: long bones, short bones, flat bones, and irregular bones. The longest bone in your body is the femur (thigh bone), which extends from your hip to your knee. It is a long bone and functions to support your weight as you stand, walk, or run. Your wrist is composed of eight irregular-shaped bones, which allow for the intricate movements of your hands. Your twelve ribs on each side of your body are curved flat bones that protect your heart and lungs. Thus, the bones’ different sizes and shapes allow for their different functions.
Bones are composed of approximately 65 percent inorganic material known as mineralized matrix. This mineralized matrix consists of mostly crystallized hydroxyapatite. The bone’s hard crystal matrix of bone tissue gives it its rigid structure. The other 35 percent of bone is organic material, most of which is the fibrous protein collagen. The collagen fibers are networked throughout bone tissue and provide it with flexibility and strength. The bones’ inorganic and organic materials are structured into two different tissue types. There is spongy bone, also called trabecular or cancellous bone, and compact bone, also called cortical bone (Figure 2.26 “The Arrangement of Bone Tissues”). The two tissue types differ in their microarchitecture and porosity. Trabecular bone is 50 to 90 percent porous and appears as a lattice-like structure under the microscope. It is found at the ends of long bones, in the cores of vertebrae, and in the pelvis. Trabecular bone tissue makes up about 20 percent of the adult skeleton. The more dense cortical bone is about 10 percent porous and it looks like many concentric circles, similar to the rings in a tree trunk, sandwiched together (Figure 2.27 “Cortical (Compact) Bone”). Cortical bone tissue makes up approximately 80 percent of the adult skeleton. It surrounds all trabecular tissue and is the only bone tissue in the shafts of long bones.
Figure 2.26 The Arrangement of Bone Tissues

Image by Gtirouflet / CC BY-SA 3.0
The two basic tissue types of bones are trabecular and cortical. This photo shows normal (left) and degraded (right) trabecular (spongy) bone.
Figure 2.27 Cortical (Compact) Bone.
Bone tissue is arranged in an organized manner. A thin membrane, called the periosteum, surrounds the bone. It contains connective tissue with many blood vessels and nerves. Lying below the periosteum is the cortical bone. In some bones, the cortical bone surrounds the less-dense trabecular bone and the bone marrow lies within the trabecular bone, but not all bones contain trabecular tissue or marrow.
Bone Tissues: Cells, Modeling and Remodeling
Bone tissue contains many different cell types that constantly resize and reshape bones throughout growth and adulthood. Bone tissue cells include osteoprogenitor cells, osteoblasts, osteoclasts, and osteocytes. The osteoprogenitor cells are cells that have not matured yet. Once they are stimulated, some will become osteoblasts, the bone builders, and others will become osteoclasts, the cells that break bone down. Osteocytes are the most abundant cells in bone tissue. Osteocytes are star-shaped cells that are networked throughout the bone via their long cytoplasmic arms that allow for the exchange of nutrients and other factors from bones to the blood and lymph.
During infancy, childhood, and adolescence, bones are continuously growing and changing shape through two processes called growth (ossification) and modeling. In fact, in the first year of life, almost 100 percent of the bone tissue in the skeleton is replaced. In the process of modeling, bone tissue is dismantled at one site and built up at a different site. In adulthood, our bones stop growing and modeling, but continue to go through a process of bone remodeling. In the process of remodeling, bone tissue is degraded and built up at the same location. About 10 percent of bone tissue is remodeled each year in adults. Bones adapt their structure to the forces acting upon them, even in adulthood. This phenomenon is called Wolff’s law, which states that bones will develop a structure that is best able to resist the forces acting upon them. This is why exercising, especially when it involves weight-bearing activities, increases bone strength.
The first step in bone remodeling is osteocyte activation. Osteocytes detect changes in mechanical forces, calcium homeostasis, or hormone levels. In the second step, osteoclasts are recruited to the site of the degradation. Osteoclasts are large cells with a highly irregular ruffled membrane. These cells fuse tightly to the bone and secrete hydrogen ions, which acidify the local environment and dissolve the minerals in the bone tissue matrix. This process is called bone resorption and resembles pit excavation. Our bodies excavate pits in our bone tissue because bones act as storehouses for calcium and other minerals. Bones supply these minerals to other body tissues as the demand arises. Bone tissue also remodels when it breaks so that it can repair itself. Moreover, if you decide to train to run a marathon your bones will restructure themselves by remodeling to be better able to sustain the forces of their new function.
After a certain amount of bone is excavated, the osteoclasts begin to die and bone resorption stops. In the third step of bone remodeling, the site is prepared for building. In this stage, sugars and proteins accumulate along the bone’s surface, forming a cement line which acts to form a strong bond between the old bone and the new bone that will be made. These first three steps take approximately two to three weeks to complete. In the last step of bone remodeling, osteoblasts lay down new osteoid tissue that fills up the cavities that were excavated during the resorption process. Osteoid is bone matrix tissue that is composed of proteins such as collagen and is not mineralized yet. To make collagen, vitamin C is required. A symptom of vitamin C deficiency (known as scurvy) is bone pain, which is caused by diminished bone remodeling. After the osteoid tissue is built up, the bone tissue begins to mineralize. The last step of bone remodeling continues for months, and for a much longer time afterward the mineralized bone is continuously packed in a more dense fashion.
Thus, we can say that bone is a living tissue that continually adapts itself to mechanical stress through the process of remodeling. For bone tissue to remodel certain nutrients such as calcium, phosphorus, magnesium, fluoride, vitamin D, and vitamin K are required.
Bone Minderal Density is an Indicator of Bone Health
Bone mineral density (BMD) is a measurement of the amount of calcified tissue in grams per centimeter squared of bone tissue. BMD can be thought of as the total amount of bone mass in a defined area. When BMD is high, bone strength will be great. Similar to measuring blood pressure to predict the risk of stroke, a BMD measurement can help predict the risk of bone fracture. The most common tool used to measure BMD is called dual energy X-ray absorptiometry (DEXA). During this procedure, a person lies on their back and a DEXA scanner passes two X-ray beams through their body. The amount of X-ray energy that passes through the bone is measured for both beams. The total amount of the X-ray energy that passes through a person varies depending on their bone thickness. Using this information and a defined area of bone, the amount of calcified tissue in grams per unit area (cm2) is calculated. Most often the DEXA scan focuses on measuring BMD in the hip and the spine. These measurements are then used as indicators of overall bone strength and health. DEXA is the cheapest and most accurate way to measure BMD. It also uses the lowest dose of radiation. Other methods of measuring BMD include quantitative computed tomography (QCT) and radiographic absorptiometry. People at risk for developing bone disease are advised to have a DEXA scan. We will discuss the many risk factors linked to an increased incidence of osteoporosis and the steps a person can take to prevent the disease from developing.
Attribution
Creative Commons Attribution 4.0 International License
This part contains content from OpenStax College, Anatomy and Physiology. OpenStax CNX. Download for free at http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@15.1.
University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
This resource has been adapted from: OpenStax Anatomy and Physiology // CC BY 4.0
- Chapter 2 The Human Body
An Introduction to Human Nutrition // CC BY-NC-SA 3.0
- Chapter 1 Basic Concepts in Nutrition
- Chapter 3 Water and Electrolytes
- Chapter 4 Carbohydrates
- Chapter 5 Lipids
- Chapter 6 Protein
- Chapter 8 Energy
- Chapter 12 Nutrition Applications
- Chapter 13 Lifespan Nutrition From Pregnancy to the Toddler Years
- Chapter 14 Lifespan Nutrition During Childhood and Adolescence
- Chapter 15 Lifespan Nutrition in Adulthood
- Chapter 17 Food Safety
- Chapter 18 Nutritional Issues
Chapters and sections were borrowed and adapted from the above existing OER textbooks on human nutrition. Without these foundational texts, a lot more work would have been required to complete this project. Thank you to those who shared before us.

SA Bos, M.D.
Lead Author